Question
In: Nursing
write a summary on the evolution of nursing: the history of nursing and nursing education, changes...
write a summary on the evolution of nursing: the history of nursing and nursing education, changes in nursing during the 20th century,significant changes,development of practical and vocational,factors that influenced practical and vocational nursing,licensure for practical and vocational,health care delivery systems,delivery of patient care,nursing care models and roles and responsibilities of vocational nursing education
Solutions
Expert Solution
ANSWER: EVOLUTION OF NURSING AS A PROFESSION
As caretakers of children, family and community, it was natural that women were the nurses, the caregivers, as human society evolved. Nursing may be the oldest known profession, as some nurses were paid for their services from the beginning. The home, in fact, was the center of health care, and for the first two centuries after European exploration of North America, all nursing was home nursing. Even when the nation’s first hospital began in Philadelphia in 1751, it was thought of primarily as an asylum or poorhouse; another century or more would pass before the public viewed hospitals as reputable and safe.
- Nursing as a practice is said to begin between 1840 and 1845. In Great Britain, Florence Nightingale led several women to a group of sick or injured Crimean War soldiers and began to give them supervised care. On the other side of the sea, American doctor Joseph Warrington wrote a book for society nurses and midwives, the first example of a regulated nursing text.
- Collectively, the volunteer nurses, often female slaves, helped save a substantial number of lives. As a result, respect for nursing grew markedly among Americans. With newfound public support and indisputable contributions to health care, the nursing profession would develop quickly.
- As time went on, hospitals grew larger and education became more comprehensive. Nurses of all races and backgrounds were accepted into programs and became part of the workforceIn the 1960s, it became commonplace for hospitals to require nurses to have a specialty instead of being proficient in several different areas.
EVOLUTION OF NURSING EDUCATION:
- In 1798 Valentine Seaman, a New York physician, organized an early course of lectures for nurses who cared for maternity patients.
- . An early nineteenth-century program, the Nurse Society of Philadelphia (also referred to as the Nurse Charity of Philadelphia) trained women in caring for mothers during childbirth and postpartum period.
- Between 1839 and 1850 the Nurse Society employed about fifty nurses, establishing an early practice of engaging nurses for care of patients in the home.
- The commendable service rendered by Civil War nurses provided a rationale for future experiments in setting up training programs for nursing. One such program was initiated in Pennsylvania where the Women’s Hospital of Philadelphia offered a six months nurse training course, which graduated its first class in 1869.
- The year 1873 was a watershed year in American professional nursing history. In that year, three nurse educational programs—the New York Training School at Bellevue Hospital, the Connecticut Training School at the State Hospital (later renamed New Haven Hospital) and the Boston Training School at Massachusetts General Hospital—began operations.
- By 1900, somewhere between 400 to 800 schools of nursing were in operation in the country
- Schools of nursing did improve over time. Better oversight of nursing educational programs by state licensing boards as well as the increasingly complex demands of patient care led the schools to increase the amount of theoretical instruction and decrease the amount of direct work performed by students.
SIGNIFICANT CHANGES IN NURSING:
- One prominent change in the evolution of the nursing profession is formalized education.
- The first training programs opened at hospitals in the late-19th century. Student nurses received clinical instruction in exchange for providing care to patients.
- By the second half of the 20th century, patient needs became more complex and hospitals required skilled nurses to manage them.
- The hospital-based education model thus declined in favor of training programs at colleges and universities.
- By 1960, over 170 college nursing programs dotted the country. Texas Woman’s University opened the state’s first nationally accredited nursing program in 1950, making it one of the oldest in Texas. Today, 871 schools in the U.S. offer nursing education programs at the undergraduate, graduate and postgraduate levels
CHANGES IN NURSING IN 20TH CENTURY :
20th century During the twentieth century nurses made tremendous advancements in the areas of:
- education
- practice
- research
- technology.
- . Nursing as a science progressed through education, clinical practice, development of theory, and rigorous research. Today nurses continue to be challenged to expand their roles and explore new areas of practice and leadership.
- Beginning in the 1960s, new types of nurses, who specialized in different hospital settings such as intensive care units, and nurse practitioners who were trained to deliver a variety of primary care services began to appear on the health care scene.
- Today, nurse practitioners, clinical nurse specialists, and other specialty-area nurses are well established and carry out a significant portion of health care activities
FACTORS THAT INFLUENCED PRACTICAL AND VOCATIONAL NURSING:
- high demand of nurses.
- to serve women as well. As women needed female health workers for their checkups
- to serve humanity.
- To help and care people
- An ideal opportunity of employment
- under the influence family and near surroundings
- It is a occupation which is needed by the society
- As it is a health-related area.
- Alone physicians were not sufficient to take care people.
- nurses bridging the gap between physician and patient.
LICENSURE FOR PRACTICAL AND VOCATIONAL NURSING:
The Licensed Practical/Vocational Nurse (LP/VN) provides direct nursing care to individuals who are in stable condition. The LP/VN also works with other health care team members in rendering care in complex situations. The LP/VN uses the Nursing Process of assessment, planning, intervention, and evaluation in the delivery of care to individuals. The term Licensed Vocational Nurse (LVN) is the recognized title in Texas and California. All other states use the title of Licensed Practical Nurse (LPN). The LP/VN designation includes both.
- Works with other health care team members in rendering care in complex situations.
- Uses Nursing Process of assessment, planning, intervention, and evaluation to deliver care.
- May render total patient care, administer medications, perform treatments, communicate with other health care team members, report information, assess individuals, plan for the delivery of care, etc.
- May focus on areas such as Pharmacology, Long-Term Care, and Infusion Therapy.
- Usually supervised by a registered nurse.
- Becomes involved with patient care at the direction of the supervising nurse, physician, or dentist.
HEALTH CARE DELIVERY SYSTEM:
Health care delivery system is defined as the aggregate of institutions, organizations and persons who enter, the health care system, Who has responsibility that, Include the promotion of health, prevention of illness, detection and treatment of disease and rehabilitation.
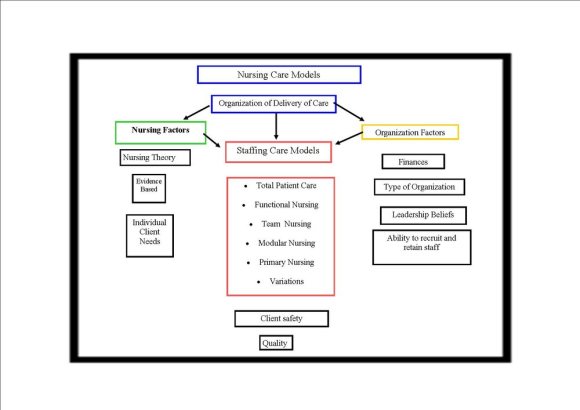
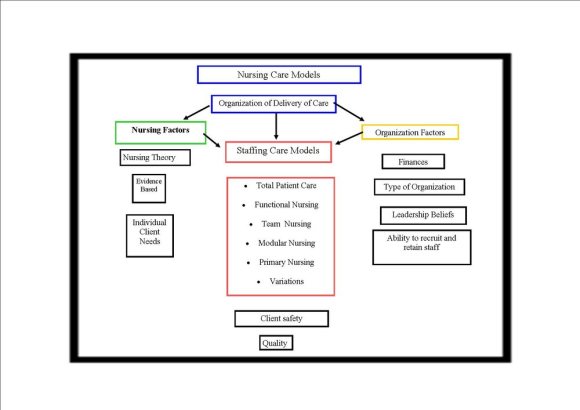
 MODELS OF NURSING
CARE:
MODELS OF NURSING
CARE:
- Various models for the delivery of nursing care such as patient allocation, primary nursing and team nursing have been implemented over the past few decades
-
The Human Caring Theory Introduced in 1979 by Dr. Jean Watson, a distinguished professor at the University of Colorado, this theory evolved from her search for the relationship between human caring and nursing
-
Primary Nursing Model Primary care nursing is when a single nurse is identified as the point of contact and primary caregiver for a patient during his or her particular hospital stay or other episode of care.
- Team-based nursing: Pairing nurses for individual patient care
- Modular nursing: Similar to the team-based approach, where the unit is divided into quadrants and teams are assigned to each.
- Functional nursing: Nurses are each assigned specific care tasks and have a single-source direct report nurse.
- Float nursing: Nurses move from unit to unit on a set schedule, or are stationed in a permanent float pool
ROLES AND RESPONSIBILITIES OF VOCATIONAL NURSING EDUCATION:
- Checking vital signs, like heart rate or blood pressure
- Updating medical histories
- Dressing wounds
- Inserting catheters
- Helping patients eat, dress, bathe, etc.
- Listening to patients and their families
- Addressing questions/concerns from patients
- Informing doctors and RNs of any issues
- Collecting lab samples
- LVNs typically work full-time and are likely to work irregular hours, such as nights and weekends, to care for patients. These nurses can work in a wide range of medical settings, including nursing care facilities, hospitals, doctors' offices, and home healthcare services.
- Assumes responsibility and accountability for designated patients
- Provides Nursing Care to all patients of all ages
- Identifies self as nurse responsible patient care to patients, family and physicians
- Provides nursing care for all patients within scope of LVN practice
- Gathers data relevant to the patient’s individual needs and age group
- Documents nursing observations according to hospital charting standards
- Reports symptoms, reactions and progress of patient to the clinical supervisor and/or charge nurse and appropriate action has been taken
- Pursues proper chain of command to attain a satisfactory solution
- Assists the RN in patient and family education
- Utilizes educational opportunities within the hospital and other avenues to maintain clinical expertise to promote personal growth and development
- Responsible for knowledge of legal aspects of nursing
- Attends fire and safety classes annually and maintains a current CPR (BLS) card
Related Solutions
write a summary on the evolution of nursing: the history of nursing and nursing education, changes...
Provide a brief summary of the history of education, special education, and special education laws. Why...
Write a summary overview of the History of Madagascar?
write a summary on the models for nursing informatics
Summary of education in Madagascar
Review the nursing journals that deal primarily with education, such as the Journal of Nursing Education,...
write a summary about your experience this term in relation to your Evolution in becoming a...
What is the National Labor Relations Act? Write a short summary of the history of this...
summary of the history of RAM memory?
4. Technology-based nursing education is the education modality for nursing today.. Do these techniques appear to...
- What’s the cost of each component of capital and which need to be adjusted? What do...
- Answer the following questions 1) How does ASC 606 — Revenue From Contracts With Customers(new standard...
- Project 7-6: Sales Tax Calculator Create a program that uses a separate module to calculate sales...
- On June 30, Sharper Corporation’s stockholders' equity section of its balance sheet appears as follows before...
- In this journal you are asked to take the role of a mayor or congressional representative...
- Answer correctly the below 25 multiple questions on Software Development Security. Please I will appreciate the...
- 1. The activation energy of a certain reaction is 41.5kJ/mol . At 20 ?C , the...
 Nightingale answered 3 years ago
Nightingale answered 3 years ago