Question
In: Nursing
Explain how a deficiency in pyruvate kinase in erythrocytes and inherited aldolase A deficiency will cause...
Explain how a deficiency in pyruvate kinase in erythrocytes and inherited aldolase A deficiency will cause hemolytic anemia.
Solutions
Expert Solution
Ans.
Pyruvate kinase deficiency is an inherited lack of the enzyme pyruvate kinase, which is used by red blood cells. Without this enzyme, red blood cells break down too easily, resulting in a low level of these cells (hemolytic anemia).
Pyruvate kinase enzyme breaks down a chemical compound called adenosine triphosphate (ATP). Because this enzyme is deficient, there is a lack of ATP. This leads to dehydration of red blood cells and abnormal red cell shapes. The altered red blood cell has a shortened lifespan leading to hemolytic anemia.
Causes
Pyruvate kinase deficiency (PKD) is passed down as an autosomal recessive trait. This means that a child must receive a non-working gene from each parent to develop the disorder.
There are many different types of enzyme-related defects of the red blood cell that can cause hemolytic anemia. PKD is the second most common cause, after glucose-6-phosphate dehydrogenase (G6PD) deficiency.
PKD is found in people of all ethnic backgrounds. But, certain populations, such as the Amish, are more likely to develop the condition.
Symptoms can be extremely varied among those suffering from pyruvate kinase deficiency. The majority of those suffering from the disease are detected at birth while some only present symptoms during times of great physiological stress such as pregnancy, or with acute illnesses (viral disorders).[7] Symptoms are limited to or most severe during childhood.[8] Among the symptoms of pyruvate kinase deficiency are:[2]
- Mild to severe hemolytic Anemia
- Cholecystolithiasis
- Tachycardia
- Hemochromatosis
- Icteric sclera
- Splenomegaly
- Leg ulcers
- Jaundice
- Fatigue
- Shortness of breath
The level of 2,3-bisphosphoglycerate is elevated: 1,3-bisphosphoglycerate, a precursor of phosphoenolpyruvate which is the substrate for Pyruvate kinase, is increased and so the Luebering-Rapoport pathway is overactivated. This led to a rightward shift in the oxygen dissociation curve of hemoglobin (i.e. it decreases the hemoglobin affinity for oxygen): In consequence, patients may tolerate anemia surprisingly well.
PathophysiologyEdit
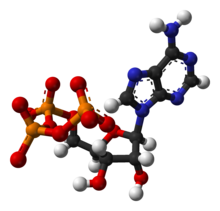
ATP-3D
Pyruvate kinase is the last enzyme involved in the glycolytic process, transferring the phosphate group from phosphenol pyruvate to a waiting adenosine diphosphate (ADP) molecule, resulting in both adenosine triphosphate (ATP) and pyruvate. This is the second ATP producing step of the process and the third regulatory reaction.[7][13] Pyruvate kinase deficiency in the red blood cells results in an inadequate amount of or complete lack of the enzyme, blocking the completion of the glycolytic pathway. Therefore, all products past the block would be deficient in the red blood cell. These products include ATP and pyruvate.[2]
Mature erythrocytes lack a nucleus and mitochondria. Without a nucleus, they lack the ability to synthesize new proteins so if anything happens to their pyruvate kinase, they are unable to generate replacement enzymes throughout the rest of their life cycle. Without mitochondria, erythrocytes are heavily dependent on the anaerobic generation of ATP during glycolysis for nearly all of their energy requirements.[14]
With insufficient ATP in an erythrocyte, all active processes in the cell come to a halt. Sodium potassium ATPase pumps are the first to stop. Since the cell membrane is more permeable to potassium than sodium, potassium leaks out. Intracellular fluid becomes hypotonic, water moves down its concentration gradient out of the cell. The cell shrinks and cellular death occurs, this is called 'dehydration at cellular level'.[2][15][16] This is how a deficiency in pyruvate kinase results in hemolytic anaemia, the body is deficient in red blood cells as they are destroyed by lack of ATP at a larger rate than they are being created.
Aldolase A deficiency, is an autosomal recessive[3] metabolic disorder resulting in a deficiency of the enzyme aldolase A; the enzyme is found predominantly in red blood cells and muscle tissue. The deficiency may lead to hemolytic anaemia as well as myopathy associated with exercise intolerance and rhabdomyolysis in some cases.
Low aldolase levels
Less than 2.0 to 3.0 U/L is considered a low level
of aldolase. Low levels of
aldolase can be seen in people with: fructose
intolerance. muscle-wasting disease. late stage muscular
dystrophy.
the symptoms of hereditary fructose intolerance?
After ingesting fructose, individuals with hereditary fructose intolerance may experience nausea, bloating, abdominal pain, diarrhea, vomiting, and low blood sugar (hypoglycemia). Affected infants may fail to grow and gain weight at the expected rate (failure to thrive).
Causes
Characterised as a recessive disorder, symptomatic presentation requires the inheritance of aldolase A mutations from both parents. This conclusion is substantiated through the continuum type presentation witnessed, wherein heterozygous parents have intermediate enzyme activity. Structural instability has been indicated in four of the patients, with particular sensitivity to increased temperature according to direct enzymatic testing. This is exemplified in the early diagnosis of hereditary pyropoikilocytosis in the Sicilian girl. Deterioration with fever is likewise congruent.[4] However, this direct relation has been disputed due to the increased overall metabolism and oxygen consumption also accompanying such maladies.[11]
Sequence analysis has been conducted for three of the patients each revealing a distinct alteration at regions of typically high conservation. The conversion of the 128th aspartic acid to glycine causes conformational change according to CD spectral analysis and thermal lability in mutagenic analysis.[3][12] Similarly the charge disruption created through the exchange of the negatively charged glutamic acid for positively charged lysine (at residue 209 of the E helix) disrupts interface interaction of the protein's subunits and therein destabilises its native tetrahedral configuration.[9] The final case is unique in its non-homozygosity. A comparable maternal missense mutation wherein tyrosine is replaced by cysteine alters the carboxy-terminus due to its proximity to a crucial hinge structure. However, the paternal nonsense mutation at arginine 303 truncates the peptide. It is notable that Arg303 is required for enzymatic activity.
Related Solutions
2. a. explain how a mutation in pyruvate dehydrogenase kinase that increases the enzymes Km will...
can aldolase B deficiency affect glucogeonesis? and why?
Explain how erythrocytes are recycled
What are structural differences between M1 pyruvate Kinase and Haemoglobin?
All the energy investment reactions involve _______. A. isomerase B. kinase C. dehydrogenase D. aldolase
What activates pyruvate kinase, what is this activation called, and why does it occur?
(Q001) Glucose-6-phosphate dehydrogenase deficiency (G6PD deficiency) is an inherited disorder where either the body has less...
What is the metabolic logic regarding stimulation of pyruvate dehydrogenase kinase (PDK) activity by ATP, whereas...
Pyruvate dehydrogenase (PDH) kinase 1 (PDK1) phosphorylates and inhibits PDH and thusly increases citrate production for...
Explain why the symptoms of fumarase deficiency are similar to the symptoms of a deficiency in...
- On June 30, Sharper Corporation’s stockholders' equity section of its balance sheet appears as follows before...
- In this journal you are asked to take the role of a mayor or congressional representative...
- Answer correctly the below 25 multiple questions on Software Development Security. Please I will appreciate the...
- 1. The activation energy of a certain reaction is 41.5kJ/mol . At 20 ?C , the...
- Give TWO pieces of evidence that you've successfully made methyl salicylate. Remember when you cite TLC...
- Describe briefly the evolution of Craniata and Vertebrata.
- How many grams are in a 0.10 mol sample of ethyl alcohol?
 Nightingale answered 3 years ago
Nightingale answered 3 years ago